Vitor Ferreira, Cintia Folgueira, María García-Altares, Maria Guillén, Mónica Ruíz-Rosario, Giada DiNunzio, Irma Garcia-Martinez, Rosa Alen, Christoph Bookmeyer, John G. Jones, Juan C. Cigudosa, Pilar López-Larrubia, Xavier Correig-Blanchar, Roger J. Davis, Guadalupe Sabio, Patricia Rada & Ángela M. Valverde.
Olanzapine (OLA), a widely used second-generation antipsychotic (SGA), causes weight gain and metabolic alterations when administered orally to patients. Recently, we demonstrated that, contrarily to the oral treatment which induces weight gain, OLA administered via intraperitoneal (i.p.) in male mice resulted in body weight loss. This protection was due to an increase in energy expenditure (EE) through a mechanism involving the modulation of hypothalamic AMPK activation by higher OLA levels reaching this brain region compared to those of the oral treatment. Since clinical studies have shown hepatic steatosis upon chronic treatment with OLA, herein we further investigated the role of the hypothalamus-liver interactome upon OLA administration in wild-type (WT) and protein tyrosine phosphatase 1B knockout (PTP1B-KO) mice, a preclinical model protected against metabolic syndrome. WT and PTP1B-KO male mice were fed an OLA-supplemented diet or treated via i.p.
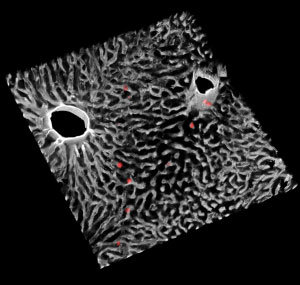
Mechanistically, we found that OLA i.p. treatment induces mild oxidative stress and inflammation in the hypothalamus in a JNK1-independent and dependent manner, respectively, without features of cell dead. Hypothalamic JNK activation up-regulated lipogenic gene expression in the liver though the vagus nerve. This effect concurred with an unexpected metabolic rewiring in the liver in which ATP depletion resulted in increased AMPK/ACC phosphorylation. This starvation-like signature prevented steatosis. By contrast, intrahepatic lipid accumulation was observed in WT mice treated orally with OLA; this effect being absent in PTP1B-KO mice. We also demonstrated an additional benefit of PTP1B inhibition against hypothalamic JNK activation, oxidative stress and inflammation induced by chronic OLA i.p. treatment, thereby preventing hepatic lipogenesis.
The protection conferred by PTP1B deficiency against hepatic steatosis in the oral OLA treatment or against oxidative stress and neuroinflammation in the i.p. treatment strongly suggests that targeting PTP1B might be also a therapeutic strategy to prevent metabolic comorbidities in patients under OLA treatment in a personalized manner.